The Canadian healthcare system was designed to be a social public healthcare system, providing care to all citizens equally. However, with the evolving times, a number of challenges have begun to hinder the system from successfully meeting the needs of Canadian residents. Using a combination of new technologies such as AI, remote monitoring devices, and blockchain technology, there is great potential to decentralize care provision and implement a more personalized and effective model of care delivery.
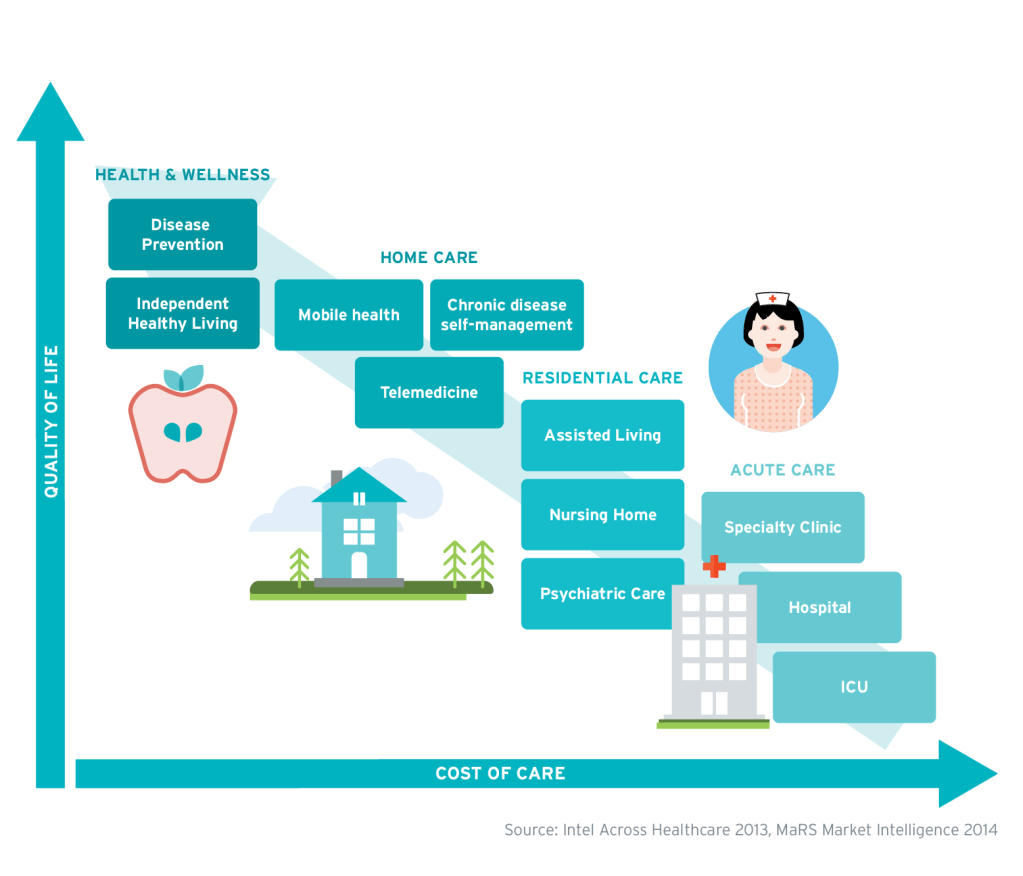
Traditional healthcare follows a centralized mechanism of care delivery, revolving around the medical facility, where complete control lies with the physician, including all patient data – there’s an inherent reliance on physicians to move forward at each stage across the continuum of care. Moreover, the cost of healthcare is rising rapidly, further limiting the healthcare system. A more decentralized model of care delivery would place patients at the center of the healthcare system, allowing physicians to deliver higher quality of care, while reducing overall costs.
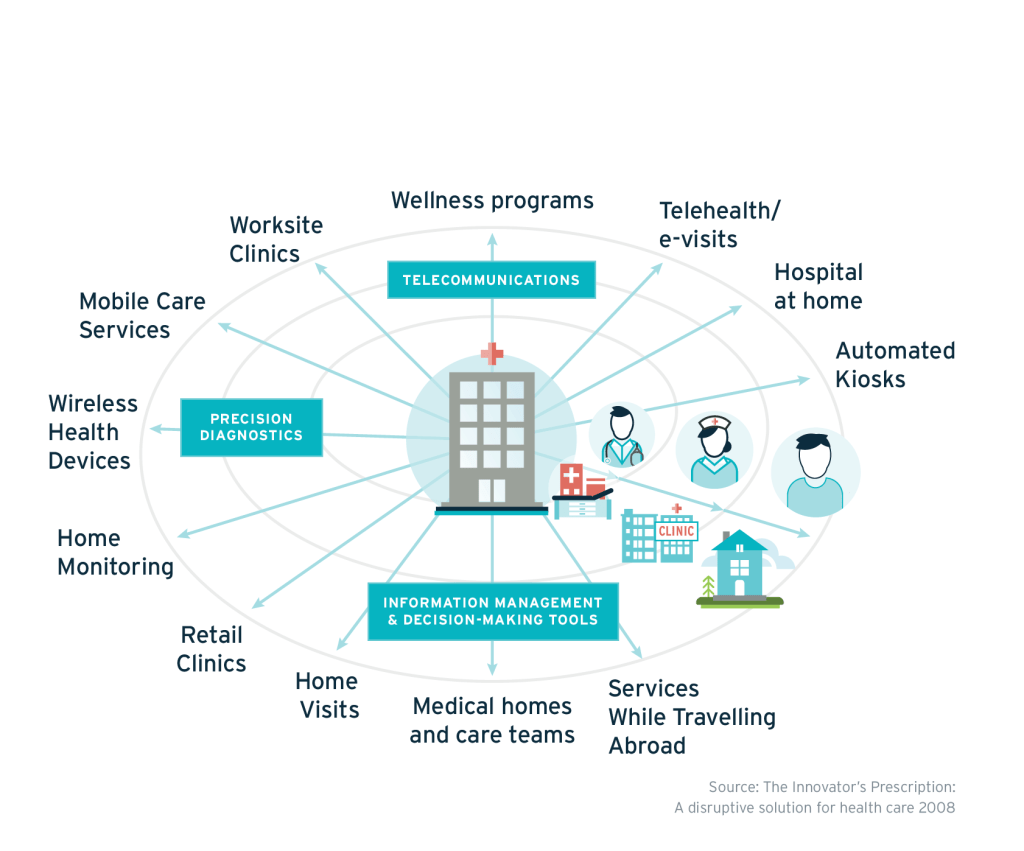
A decentralized model of healthcare relies on two main pillars, the first of which is ‘community based healthcare’. This model makes patients the center of the healthcare system, and takes care provision from medical facilities to patient homes. This is powered through tele-health i.e. patients and doctors connecting via video call on a phone app to power a consultation. This is a very effective method of patient – physician interactions, curbing the cost of healthcare, and making physician care accessible and flexible. Moreover, it allows patients to untie themselves from a particular medical facility, and instead have access to a number of doctors.
The second pillar – ‘connected healthcare’ – leverages technology to enable data and information flow through a decentralized healthcare system. In effect, it augments to the community based healthcare model by providing access to patient data during a tele-health consult, ensuring informed diagnosis and care plans. Connected healthcare is driven by the use of remote monitoring medical devices such as point of care diagnostics, wireless devices to measure health indicators, and fitness trackers. This allows for the collection of holistic medical data points encompassing both physiological (such as blood pressure, heart rate, and temperature) and physical (step count, sleep patterns, activity levels) patient data. These devices are usually Bluetooth enabled and are able to transmit information wirelessly to the cloud where it can be stored until required. Further, these data points can be available to physicians during a tele-health consults, allowing for a more personalized, informed conversation.
Another important aspect of decentralizing healthcare is the flow of sensitive patient information such as patient’s electronic medical records (EMRs). There is an opportunity to leverage blockchain to store EMRs. This would alleviate security and privacy concerns, as every healthcare transaction would be recorded on an EMR blockchain network. Currently, one of the largest concerns related to telemedicine is maintaining the privacy of patient data; healthcare facilities storing such data have to get certified by governing bodies like HIPAA to ensure they have the required security standards. With the implementation of blockchain, each addition to a patient’s medical record, by any physician, would be recorded in a secure, transparent way, with no possibility of data-tampering.
Finally, the use of artificial intelligence (AI) can further streamline and enhance care delivery. Digital assistants or chatbots using natural language processing can help doctors triage patients, freeing up their time to spend on personalized patient care, instead of repetitive tasks.
So, who is capturing the value generated from decentralization?
The simple answer is: everyone.
A number of studies confirm that accessibility to telemedicine is very beneficial to patients, particularly vulnerable segments like senior citizens and disabled people. This is because telemedicine enables easier chronic disease management and results in fewer missed appointments. Moreover, the data collected from connected health allows doctors to proactively advice on preventative health measures, and ultimately allows physicians to deliver better outcomes, while patients increase long-term quality of life.
Further, both Medical facilities and the government would see significant cost savings through the use of telemedicine as the first step in screening. This is largely because ERs will not be crowded with patients that could have been diagnosed remotely, freeing up bed space and resources for treating other patients.
Another stakeholder, not discussed much up till now – insurers – also reap some benefit of decentralization, particularly in the form of reduced medical claims. With telemedicine allowing for a more preventative approach to healthcare, patients are likely to stay healthier longer, ultimately reducing the cost insurers incur as well.
Where are we today?
Decentralizing healthcare is a great example of architectural innovation, since it not only requires the implementation of the aforementioned new technologies, but also presents the opportunity to rethink the business model for health.
Telemedicine and connected health bring with increased accessibility to care, and also the opportunity to explore a subscription-fee based business model. Much like a SaaS platform model, patients could pay a subscription fee to access digital health tools on an application, from video and messaging connectivity with doctors, to follow-ups, EMRs, and digital triaging; this is just the beginning. Health risk assessments, wellness tools, and fitness trackers open the door to a world of preventative health care. However, for the moment, this is a utopian view of what social healthcare could be if we fully leveraged the technology we have access to, and redesigned the healthcare system keeping patients at the center.
Today, a number of healthcare startups are attempting to decentralize care provision through telemedicine, digital health tools, and employee wellness platforms, primarily targeted towards employers. As we take a baby steps towards a better, more efficient healthcare system, joint leaps can be made once the government is bought in and policy experts begin to focus on healthcare.